Is Endometriosis Genetic or Hereditary?
Endometriosis, a painful and often misunderstood condition, affects millions of individuals worldwide, primarily those assigned to females at birth. While the exact cause of endometriosis remains elusive, researchers have long debated the role of genetics in its development. In this blog post, we delve into the question: Is Endometriosis Genetic or Hereditary?
What is endometriosis?
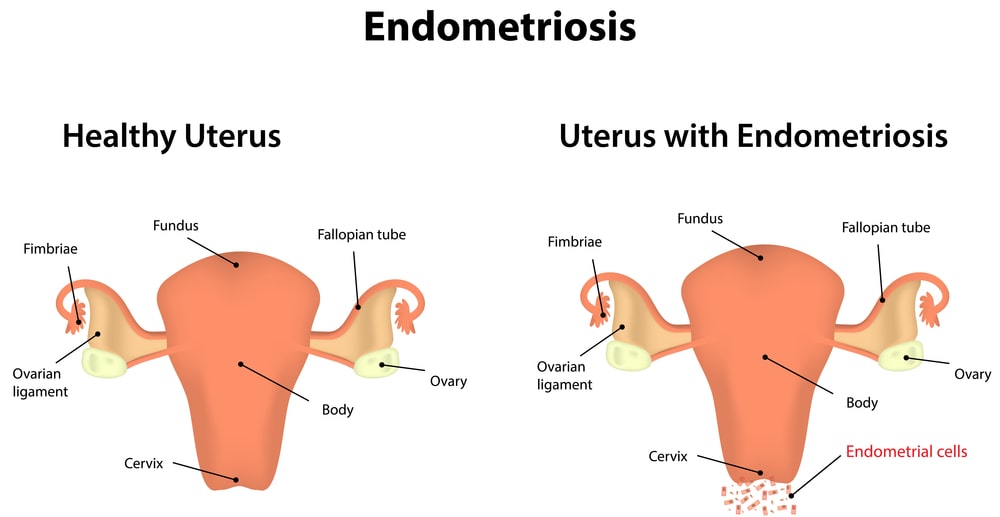
Endometriosis is a chronic and often painful condition in which tissue similar to the lining of the uterus, known as the endometrium, grows outside the uterus. This tissue can be found in various organs within the pelvic region, such as the ovaries, fallopian tubes, the outer surface of the uterus, and the lining of the pelvic cavity. In rare cases, it can also occur in other body areas.
During the menstrual cycle, the endometrial-like tissue outside the uterus responds to hormonal changes, thickening, breaking down, and bleeding, just like the normal endometrium. However, because this tissue has no way to exit the body like menstrual blood, it becomes trapped, leading to inflammation, pain, and the formation of scar tissue (adhesions).
Endometriosis can cause a range of symptoms, including Pelvic pain, Heavy menstrual bleeding (Menorrhagia), Painful periods (Dysmenorrhea), Painful intercourse (Dyspareunia), Infertility, etc.
What causes endometriosis?
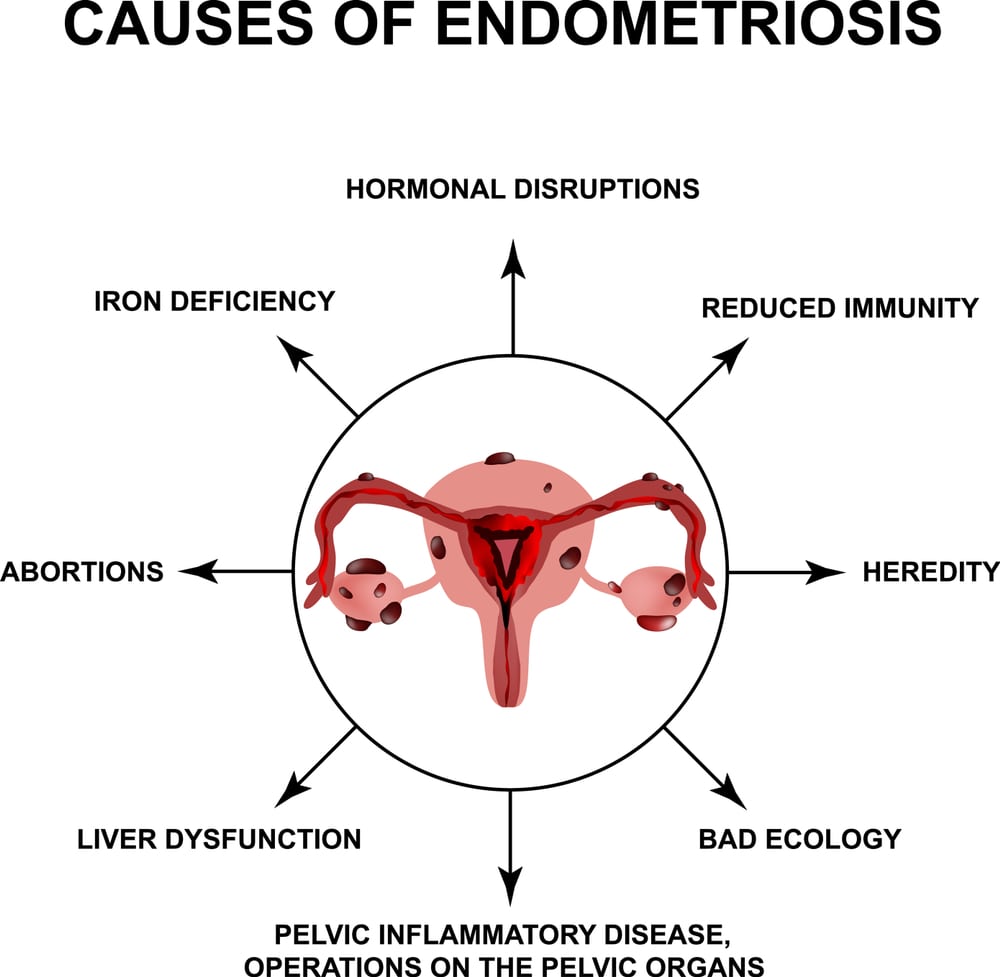
The exact cause of endometriosis remains unclear, but several theories have been proposed to explain its development. These include:
- Retrograde Menstruation: One of the most widely accepted theories suggests that during menstruation, some of the menstrual blood containing endometrial cells flows backward through the fallopian tubes into the pelvic cavity instead of exiting the body.
- Embryonic Cell Transformation: Another theory proposes that embryonic cells, which are present in the pelvic cavity from birth, can transform into endometrial-like tissue in response to hormonal signals.
- Immune System Dysfunction: It’s believed that abnormalities in the immune system may contribute to the development of endometriosis.
- Hormonal Imbalances: Factors such as early onset of menstruation, short menstrual cycles, or prolonged exposure to estrogen (such as in hormone replacement therapy) may increase the risk of developing endometriosis.
- Genetic Factors: There is evidence to suggest that genetics play a role in predisposing individuals to endometriosis.
- Environmental Factors: Exposure to certain environmental toxins, such as dioxins and endocrine-disrupting chemicals found in pesticides and plastics, has been linked to an increased risk of endometriosis.
The list can help to understand the question of the blog: is endometriosis genetic?
Signs of endometriosis:
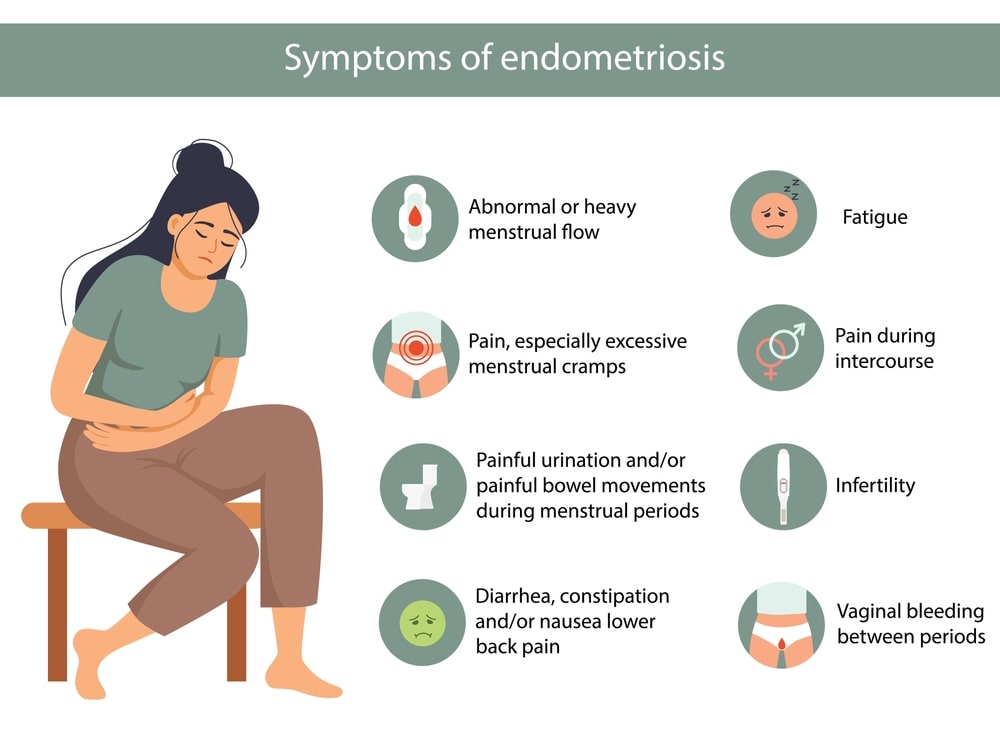
Some common signs and symptoms of endometriosis include:
- Pelvic Pain.
- Dysmenorrhea
- Heavy Menstrual Bleeding.
- Painful Intercourse (Dyspareunia).
- Chronic Pelvic Pain.
- Pain with Bowel Movements or Urination.
- Infertility
- Fatigue
- Lower Back Pain.
- Leg pain.
- Cough up blood during menstruation (rare).
- Digestive issues such as diarrhea, and constipation.
How is endometriosis diagnosed?

Here are the primary methods used for diagnosis:
- Medical History and Symptom Assessment: The healthcare provider will begin by discussing your medical history and symptoms. They will ask about your menstrual cycles, pain patterns, and any other symptoms you may be experiencing, such as pelvic pain, painful periods, painful intercourse, or infertility.
- Pelvic Examination: A pelvic examination may be performed to check for any abnormalities, such as tender areas, masses, or nodules, that could indicate the presence of endometriosis. However, it’s important to note that endometriosis lesions are not always palpable during a pelvic exam, especially if they are small or located deep within the pelvis.
- Imaging Studies: Imaging tests such as ultrasound or magnetic resonance imaging (MRI) may be recommended to visualize the pelvic organs and detect any abnormalities, such as ovarian cysts (endometriomas) or adhesions, that could suggest the presence of endometriosis. While these tests can provide valuable information, they are not definitive for diagnosing endometriosis and may not detect all cases of the disease.
- Laparoscopy: It is a minimally invasive surgical procedure performed under general anesthesia. During laparoscopy, a thin, lighted tube with a camera (laparoscope) is inserted through a small incision in the abdomen, allowing the surgeon to visualize the pelvic organs directly. If endometriosis is suspected based on symptoms or imaging findings, the surgeon may also take tissue samples (biopsies) for further examination to confirm the diagnosis.
- Biopsy and Histological Examination: Tissue samples obtained during laparoscopy are sent to a pathology laboratory for histological examination. A pathologist examines the tissue under a microscope to confirm the presence of endometrial-like glands and stroma characteristic of endometriosis.
Is endometriosis genetic?

Endometriosis does appear to have a genetic component, although the exact genetic mechanisms underlying the condition are still being researched. Evidence from family and twin studies suggests that individuals with a family history of endometriosis are at an increased risk of developing the condition themselves.
Studies have identified certain genetic variations that may be associated with increased susceptibility to endometriosis. This can help to understand: whether is endometriosis genetic. These genetic variations may affect factors such as hormone metabolism, inflammation, immune response, and cell adhesion, all of which are believed to play roles in the development and progression of endometriosis.
One of the most notable genetic variants associated with endometriosis is found in the gene known as FN1 (Fibronectin 1). This gene plays a role in cell adhesion and migration, processes that are dysregulated in endometriosis. Variations in FN1 may increase the risk of developing endometriosis by altering cellular functions within the pelvic cavity.
The relation between whether is endometriosis genetic or not is explained via some pointers below which help to relate:
Epigenetics:
It is the study of changes in gene expression or cellular phenotype caused by mechanisms other than changes in the underlying DNA sequence. These changes can be influenced by various factors such as environmental exposures, lifestyle choices, and developmental stages
In addition to genetic variations, epigenetic factors may also influence endometriosis risk. Epigenetics refers to changes in gene expression that occur without alterations to the underlying DNA sequence. Environmental factors such as exposure to certain chemicals or hormones can modify gene expression patterns, potentially contributing to the development of endometriosis.
Future Directions:
While significant progress has been made in uncovering the genetic basis of endometriosis, much remains to be understood. Further research is needed to elucidate the complex interplay between genetic predisposition, environmental factors, and the development of the condition. By unraveling these mechanisms, researchers hope to identify novel therapeutic targets and improve diagnostic strategies for endometriosis.
It’s important to note that genetics are just one piece of the puzzle when it comes to endometriosis. The condition is complex, and other factors such as hormonal imbalances, immune dysfunction, environmental exposures, and lifestyle factors may also contribute to its development. Hence, this clears the big question: is endometriosis genetic?
How to treat endometriosis?

Treatment options for endometriosis may include:
- Pain Medication: Over-the-counter pain relievers such as nonsteroidal anti-inflammatory drugs (NSAIDs) like Ibuprofen or Naproxen can help alleviate menstrual cramps and pelvic pain associated with endometriosis. For severe pain, stronger prescription medications may be necessary.
- Hormonal Therapy: Hormonal therapy aims to suppress ovulation and reduce estrogen levels, which can help alleviate symptoms and slow the growth of endometriosis lesions. Hormonal therapy options include Oral contraceptives (birth control pills), Progestins, Danazol, Gonadotropin-releasing hormone (GnRH) agonists, and antagonists, etc.
- Surgical Management: Surgery may be recommended for individuals with severe symptoms, significant endometriosis lesions, or those who do not respond to conservative treatments. Surgical options include Laparoscopic excision, Laparoscopic ablation, and Hysterectomy.
- Fertility Treatment: For individuals with endometriosis-related infertility, assisted reproductive technologies (ART) such as in vitro fertilization (IVF) may be recommended. IVF involves fertilizing eggs outside the body and transferring embryos into the uterus, bypassing the fallopian tubes affected by endometriosis.
- Complementary Therapies: Some individuals find relief from symptoms through complementary therapies such as acupuncture, dietary modifications, physical therapy, and stress management techniques.
Natural remedies for endometriosis:

Here are some natural remedies that may offer relief for individuals with endometriosis:
- Dietary Changes: Consider incorporating more fruits, vegetables, whole grains, and omega-3 fatty acids (found in fatty fish, flaxseeds, and walnuts) into your diet. Limiting processed foods, red meat, dairy, caffeine, and alcohol may also be beneficial.
- Herbal Supplements: Some herbs may have anti-inflammatory or hormone-balancing effects that could help manage symptoms of endometriosis. Examples include Turmeric, Ginger, Chamomile, and Evening primrose oil.
- Acupuncture: Acupuncture involves inserting thin needles into specific points on the body to stimulate energy flow and promote healing. Some individuals with endometriosis find acupuncture helpful in reducing pain and improving overall well-being.
- Exercise: Regular exercise can help reduce inflammation, alleviate stress, and improve circulation, which may help manage symptoms of endometriosis. Low-impact exercises such as walking, swimming, yoga, and cycling are generally recommended.
- Heat Therapy: Applying heat to the abdomen or lower back can help relax muscles and relieve menstrual cramps associated with endometriosis. Use a heating pad, or warm towel, or take a warm bath to soothe discomfort.
- Pelvic Floor Therapy: Pelvic floor physical therapy may be beneficial for individuals with endometriosis-related pelvic pain. A pelvic floor physical therapist can teach exercises and techniques to help relax and strengthen pelvic floor muscles, alleviate pain, and improve pelvic function.
Endnote:
In conclusion, while endometriosis has a strong genetic component, its development is influenced by a complex interplay of genetic, hormonal, environmental, and immune factors. Understanding the genetic underpinnings of endometriosis is crucial for developing targeted therapies and personalized treatment approaches.
Moving forward, continued research into the genetic mechanisms of endometriosis and its interaction with other factors will be essential for improving diagnostic methods, treatment options, and ultimately, the quality of life for individuals living with this debilitating condition.
FAQs:
Can you get pregnant with endometriosis?
Endometriosis may harm the egg. Alternatively, it may result in inflammation, which might disrupt the delicate hormonal balance required for women to conceive or get pregnant.
Can endometriosis cause cancer?
Women with endometriosis are more likely to develop several uncommon forms of ovarian cancer, such as endometrioid and clear-cell ovarian cancers. However, the risk is still less than 1% even with those cancer kinds.
Can endometriosis cause infertility?
It may be more difficult to become pregnant if you have endometriosis. 30–50% of individuals with endometriosis can become infertile. Individuals without endometriosis typically have a monthly probability of 10–20%, but those with endometriosis who have been medically diagnosed often have a monthly probability of 1–10%.
Can endometriosis cause weight gain?
When endometriosis causes severe bloating, also referred to as “endo belly,” it can appear as though you have gained weight. Fluid retention in endometriosis patients can cause them to gain weight.
Is endometriosis cancer?
No, endometriosis is not a cancer. While endometriosis can cause significant pain and discomfort, it is a benign condition and is not considered a form of cancer. However, some research suggests that women with endometriosis may have a slightly higher risk of certain types of ovarian cancer compared to women without the condition, but the overall risk is still low. Hence, it can clear the question: is endometriosis cancer, or is endometriosis genetic.

