Is Psoriasis Genetic?
Psoriasis is a chronic autoimmune disorder characterized by the rapid growth of skin cells, resulting in thickened, red patches covered with silvery scales. These patches can occur anywhere on the body but are most found on the elbows, knees, scalp, and lower back.
Psoriasis is a dermatological concern and can significantly impact a person’s quality of life due to discomfort, itching, and self-consciousness about the visible symptoms.
Is Psoriasis genetic? While the exact cause of psoriasis remains unclear, genetic predisposition is widely recognized as a significant factor in its development. Family studies have shown that individuals with a family history of psoriasis have a higher risk of developing the condition themselves.
Furthermore, twin studies have demonstrated a higher concordance rate of psoriasis among identical twins than fraternal twins, highlighting the strong influence of genetic factors.
What is Psoriasis?

Psoriasis is a chronic autoimmune condition that affects the skin, causing the rapid buildup of skin cells. This buildup results in thick, red patches, often covered with silvery scales, which can be itchy and painful. These patches can occur anywhere on the body but are most found on the elbows, knees, scalp, and lower back.
The exact cause of psoriasis is not fully understood, but it is believed to involve a malfunction in the immune system, which causes the skin cells to grow too quickly. Genetics and environmental factors also play a role in its development. Psoriasis can vary in severity, with some experiencing mild symptoms that come and go, while others may have severe and persistent symptoms.
While there is no cure for psoriasis, various treatments can help manage the symptoms and improve the quality of life for those affected. These treatments include topical creams and ointments, oral medications, light therapy, and in severe cases, biologic drugs that target the immune system.
Additionally, lifestyle changes such as stress management, maintaining a healthy diet, and avoiding triggers can also help in managing the condition. Is psoriasis genetic? Understanding the genetic component of psoriasis is crucial in tailoring treatments to individual needs and developing effective strategies for long-term management.
What causes Psoriasis?
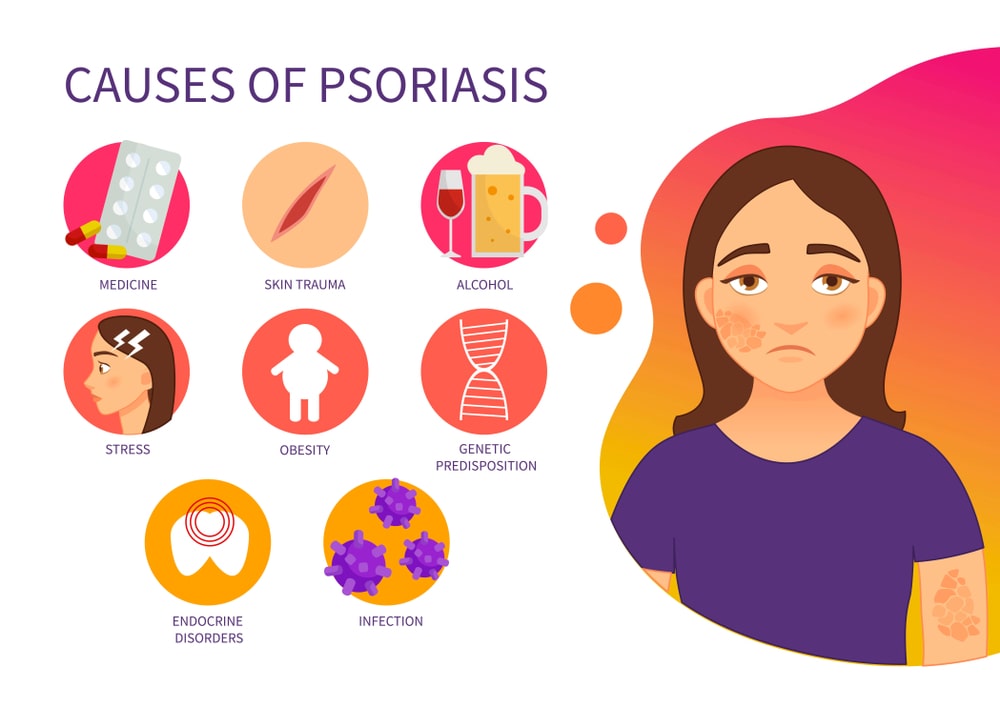
The exact cause of psoriasis is not fully understood, but it is believed to be a result of a combination of genetic, immune system, and environmental factors.
Here’s a breakdown of these factors:
- Genetics: Psoriasis tends to run in families, suggesting a genetic predisposition. Certain genetic variations have been linked to an increased risk of developing psoriasis. However, not everyone with these genetic traits will develop the condition, indicating that other factors also play a role.
- Immune System Dysfunction: Psoriasis is considered an autoimmune disease, where the immune system mistakenly attacks healthy cells in the body, in this case, skin cells. In a person with psoriasis, the immune system is overactive, leading to inflammation and the rapid production of skin cells.
- Environmental Triggers: Common triggers include stress, infections (such as streptococcal throat infections), injury to the skin (such as cuts, scrapes, or sunburns), certain medications (like lithium, beta-blockers, or antimalarial drugs), and smoking.
- Lifestyle Factors: Lifestyle choices such as smoking, excessive alcohol consumption, obesity, and a poor diet high in processed foods and sugars may also contribute to the development or worsening of psoriasis symptoms.
Is psoriasis genetic? Overall, while the exact cause of psoriasis remains unclear, it is likely a complex interplay of genetic susceptibility, immune system dysfunction, and environmental triggers. Understanding these factors can help in managing the condition effectively.
Is Psoriasis genetic?
Yes, psoriasis does have a genetic component. While not everyone with a family history of psoriasis will develop the condition, having a close relative with psoriasis increases the risk of developing it. Research suggests that multiple genes contribute to the risk of developing psoriasis, and inheriting certain combinations of these genes can predispose individuals to the condition.
The exact genetic mechanisms involved in psoriasis are complex and not fully understood. However, genetic studies have identified specific gene variants associated with psoriasis susceptibility, particularly those involved in regulating the immune system and skin cell growth.
These genetic predispositions, combined with environmental factors and immune system dysregulation, contribute to the development of psoriasis in susceptible individuals. Overall, while genetics play a significant role in psoriasis, environmental factors and immune system dysfunction also contribute to its onset and severity.
How to cure Psoriasis permanently?

There is no known cure for psoriasis. However, various treatments can help manage the symptoms and improve the quality of life for individuals affected by the condition. These treatments aim to reduce inflammation, slow down the growth of skin cells, and alleviate symptoms such as itching and discomfort.
Some common treatment options include:
- Topical Treatments: These include corticosteroids, vitamin D analogs, retinoids, coal tar, and moisturizers. They are used directly on the affected skin to lower down inflammation and scale formation.
- Phototherapy (Light Therapy): This involves exposing the skin to ultraviolet (UV) light under medical supervision. UVB phototherapy and PUVA (psoralen plus ultraviolet A) therapy are common forms of light therapy used to treat psoriasis.
- Oral Medications: In cases of moderate to severe psoriasis, oral medications such as Methotrexate, Cyclosporine, Acitretin, or Apremilast may be prescribed to suppress the immune system and reduce inflammation.
- Biologic Therapies: Biologic drugs, including TNF-alpha inhibitors, interleukin inhibitors, and other targeted therapies, are injected or infused to target specific parts of the immune system involved in the development of psoriasis.
- Lifestyle Modifications: Maintaining a healthy lifestyle, including regular exercise, stress management techniques, avoiding triggers such as smoking and excessive alcohol consumption, and following a balanced diet, may help in managing psoriasis symptoms.
While these treatments can effectively control psoriasis symptoms for many people, it’s essential to work closely with a healthcare provider to develop a personalized treatment plan. Additionally, ongoing research into the underlying causes of psoriasis may lead to new and more effective treatment options in the future.
FAQs:
Is Psoriasis contagious?
No, psoriasis is not contagious. It is an autoimmune condition caused by genetic, immune system, and environmental factors, leading to the rapid growth of skin cells and inflammation. Unlike infections or contagious diseases, psoriasis cannot be spread through physical contact, such as touching or skin-to-skin contact. People with psoriasis can safely interact with others without fear of transmitting the condition.
Is Psoriasis an Autoimmune Disease?
Yes, psoriasis is classified as an autoimmune disease. In autoimmune diseases, the immune system mistakenly attacks healthy cells and tissues in the body. In psoriasis, this immune system dysfunction leads to inflammation and the rapid turnover of skin cells, resulting in the characteristic symptoms of thickened, red patches with silvery scales. While the exact cause of psoriasis is not fully understood, immune system dysregulation is a central feature of the condition.
What does Plaque Psoriasis look like?
Plaque psoriasis typically appears as raised, red patches of skin covered with silvery-white scales, known as plaques. These plaques often develop on the elbows, knees, scalp, and lower back, but can also occur on other areas of the body. The patches can vary in size and shape and may be itchy, painful, or both. In some cases, plaque psoriasis can cause cracking and bleeding of the skin.
Is Psoriasis Dangerous?
Psoriasis itself is not considered dangerous to one’s overall health, but it can significantly impact quality of life due to its chronic nature and potential for discomfort. However, severe cases of psoriasis may increase the risk of developing other health conditions such as psoriatic arthritis, cardiovascular disease, obesity, and depression.
Additionally, certain treatments for psoriasis, particularly systemic medications, may carry risks and side effects, so it’s important for individuals with psoriasis to work closely with healthcare providers to manage their condition effectively.
What is the difference between Eczema and Psoriasis?
Eczema and psoriasis are both chronic skin conditions, but they have distinct differences. Eczema, also known as atopic dermatitis, typically appears as inflamed, itchy, red patches of skin that may ooze or crust over. It often begins in infancy or childhood and is associated with allergies and asthma.
Psoriasis, on the other hand, presents as raised, red patches with silvery scales, and tends to occur on the elbows, knees, scalp, and lower back. It is an autoimmune condition with a genetic predisposition and is not typically associated with allergies.
Additionally, eczema is more likely to flare up in response to allergens or irritants, while psoriasis flares may be triggered by stress, infections, or injury to the skin. So, is psoriasis genetic? Understanding the genetic component of psoriasis is crucial in tailoring treatments to individual needs and developing effective strategies for long-term management.